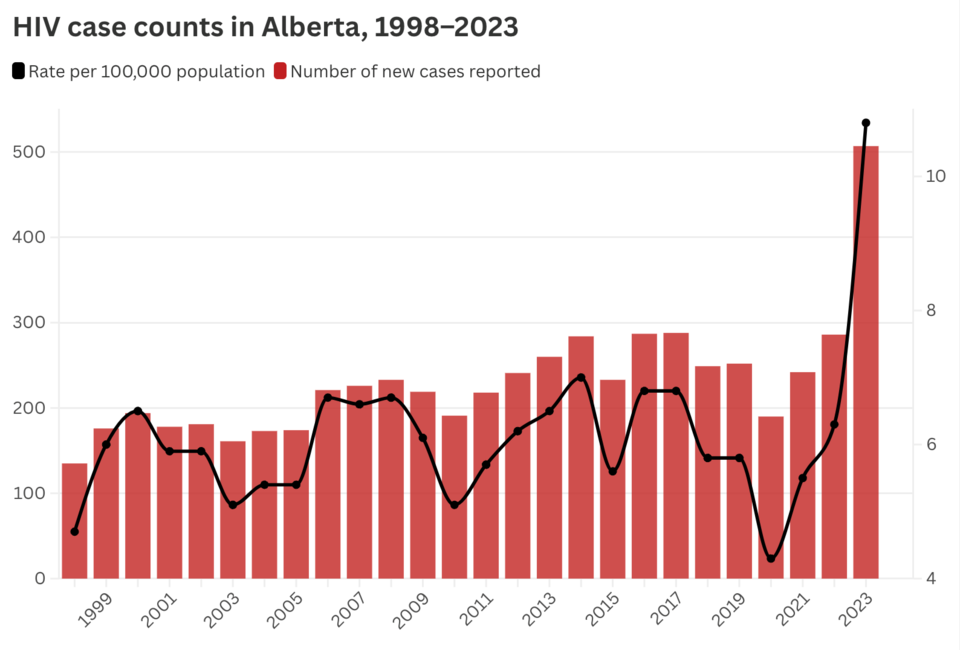
Alberta reported a record number of new HIV infections in 2023, and doctors says the surge in cases has had unexpected impacts on HIV programs in the province.
There were 507 cases of HIV reported in 2023, 73 per cent more than in 2022 and the largest year-over-year increase since HIV was included in the province’s reportable disease surveillance in 1998.
The most common cause of exposure for both men and women, according to Alberta Health, is categorized as “acquired out of country,” but experts say they are also concerned about rising in-community transmission.
“Most of the new diagnoses, the new cases we're seeing in Alberta, are actually transfers in from elsewhere. Mainly, but not always, on treatment and previously diagnosed,” said Dr. John Gill, medical director of the Southern Alberta HIV Clinic.
The influx of new patients is largely related to the population increase through federal immigration and refugee policies, Gill said.
“Many of these patients are delightful,” and their illness has often been well managed and only require a transfer of care to keep them on medication and stay non-infectious to sexual partners, he said.
But many people still require proper intake assessment, treatment for co-occurring infections, and help to be connected with necessary social supports, especially those coming from unstable or war-torn regions where access to consistent medical care is likely limited. The arrival of so many new patients in such a short time has created strains for some clinics, even though Alberta’s HIV system has run well for over 30 years, Gil said.
“It has a major unexpected effect on HIV programming, because a dramatic and unexpected increase in numbers due to a federal policy certainly puts pressure on finding adequate healthcare workers skilled to provide ongoing support for such patients,” he said.
Gill said his clinic was caught off guard by the sudden rise in the number of patients needing care.
“I'm unaware of any communication coming to my level, as medical director of the HIV clinic, that we could anticipate a large number of new, often well-managed HIV patients to be arriving. Whether Alberta Health was notified by the federal government that this would be an impact on the provincial health care budget is unclear to me,” he said.
Treatment for HIV is effective, but it is also lifelong and expensive, Gill said, and resources are needed to ensure adequate care is available.
With 54 per cent of reported HIV cases being acquired out of country, the rise in patients who are new to Alberta is only half the story, says Katie Ayres, executive director of SafeLink Alberta.
The second most common category of exposure in 2023, accounting for 19 per cent of new cases, was transmission between heterosexual partners.
“HIV, historically, has been thought of as more for gay men, or men who have sex with men, and that's certainly not the case. And it’s not what we're seeing in our HIV rates anymore and haven't for at least a decade now,” Ayres said.
The rising rates of HIV among heterosexual folks speaks to the changes around HIV education in the last few decades since effective treatment has become more available, she said.
The annual Sex Lives report from LetsStopAids surveyed Canadians aged 18–24 and found “significant deficiencies in sexual health education and awareness.”
A vast majority of young Canadians, 96 per cent, said they weren’t very familiar with sexually transmitted infection or HIV disclosure laws. The report said ignorance of these laws was contributing to Canada being the only G7 country with a rising HIV rate. Seven out of ten young people surveyed said they had never had an STI test and two-thirds said they only inconsistently used condoms. One in five reported they never use condoms.
The reasons why these trends exist among youth are anecdotal, but the survey found that age group to be less comfortable having discussions around STI and HIV disclosure or condom negotiation, Ayres noted.
“So I think there's more education that needs to be done, especially with young adults as well, and with more specific focus on the heterosexual folks too,” she said.
The number of HIV exposures related to intravenous drug use dropped in 2023 compared to the previous year, but Ayres said the ongoing opioid and drug poisoning crisis is exacerbating HIV rates and that strengthening access to supervised consumption sites, needle exchanges, and education programs for people who use drugs would help reduce transmission.
The Office of the Minister of Health said in a statement that many jurisdictions in Canada have observed increases in STIs in the last decade, and that the province supports various treatment and prevention programs.
“Alberta's government continues to work with Alberta Health Services (AHS) and community-based organizations to improve health, reduce barriers to sexually transmitted and blood-borne infections (STBBI) testing and treatment, and increase access to prenatal syphilis screening,” a spokesperson for Alberta Health said.
“Through Budget 2024, Alberta's government is continuing to provide over $7 million annually to various organizations across the province for STBBI prevention, testing and treatment, and to support wraparound services for people in vulnerable situations who are diagnosed with these infections.”